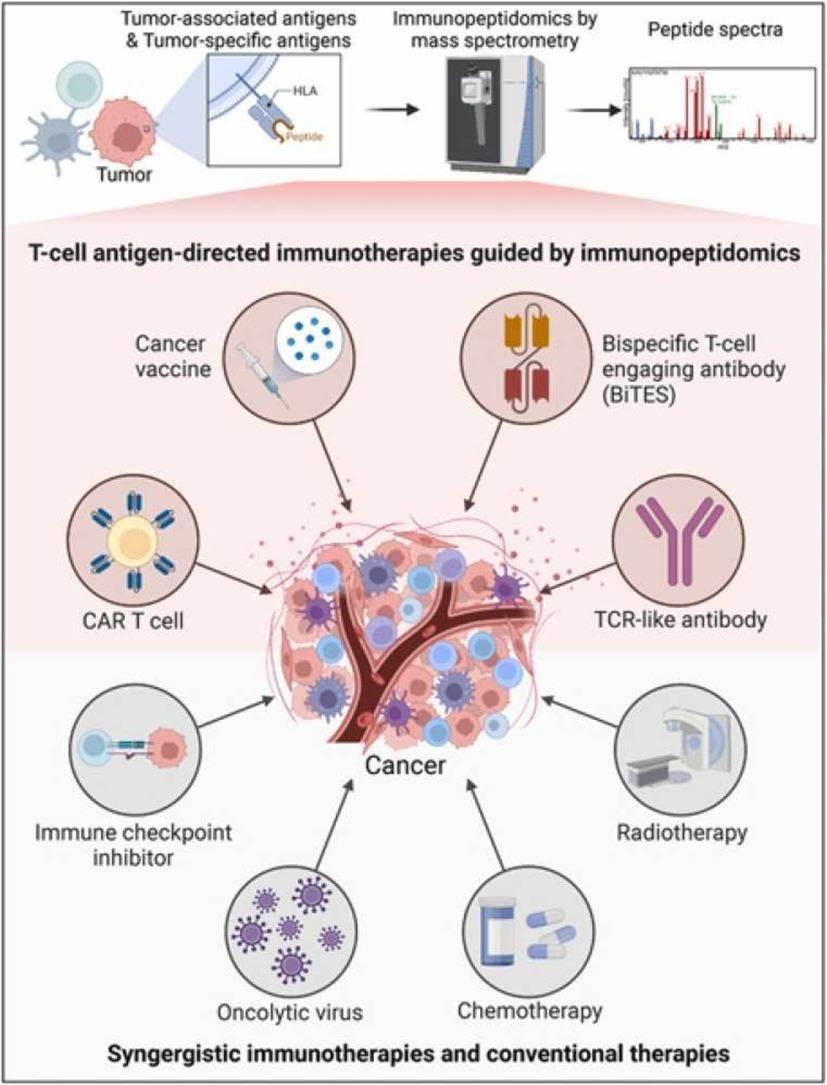
Cancer is a daunting diagnosis; however, the rapid advancements in oncology are continuously perfecting patient outcomes and quality of life. Among the groundbreaking developments, cancer vaccines are a promising frontier1. These vaccines are transforming how we approach cancer treatment, leveraging the body's immune system to fight malignancies more effectively. To grasp how cancer vaccines work, it is pivotal to understand two fundamental components of the immune system: antigens and antibodies.
Antigens are molecules or molecular structures that evoke an immune response when identified as foreign by the body's immune system. They are generally proteins or polysaccharides found on the surface of pathogens, such as viruses, bacteria, or cancer cells. In the environment of cancer, antigens may be specific to tumor cells and are known as tumor-specific antigens (TSAs) or tumor-associated antigens (TAAs).
Antibodies, also known as immunoglobulins, are proteins produced by B-cells, a type of white blood cell. They recognize and bind to specific antigens, marking the pathogen or abnormal cells (like cancer cells) for destruction by other immune cells. This antigen-antibody binding is a critical mechanism used by our immune system to target and eliminate threats effectively.
Cancer vaccines are designed to stimulate the immune system to recognize and attack cancer cells, analogous to how traditional vaccines work against infectious diseases. The development principle of cancer vaccines usually includes the identification of antigens (generally involves tumor antigen research services offered by professional organizations or CRO companies), vaccine formulation, immune activation, and targeting of cancer cells. The Vaccines can be formulated using various platforms, including:
·Peptide/Protein Vaccines: Short sequences of the target antigen are synthesized and administered to patients.
·DNA/RNA Vaccines: Genetic material encoding the target antigen is delivered to patient cells, enabling the production of the antigen within the body.
·Cell-Based Vaccines: Tumor cells or immune cells are modified to present the target antigens and stimulate an immune response. Applications of cell-based cancer vaccines are typically used in prostate cancer, lung cancer, pancreatic cancer, breast cancer, etc.
Applications and Functions of Cancer Vaccines
Cancer vaccines serve several purposes in oncology. For illustration, the HPV vaccine helps prevent cervical cancer by targeting the human papillomavirus. Provenge, a therapeutic vaccine for metastatic prostate cancer that has demonstrated a survival benefit in clinical trials, is approved for treating metastatic prostate cancer.
The field of cancer vaccines is fleetly evolving. Current research focuses on improving vaccine platforms, identifying new tumor antigens, and combining vaccines with other immunotherapies for synergistic effects. The results so far are promising, with several clinical trials showing enhanced survival rates and tumor regression. The HPV Vaccine is One of the most successful preventive cancer vaccines, reducing the incidence of cervical cancer significantly.
Conclusion
Cancer vaccines represent a paradigm shift in oncology, offering new avenues for prevention, treatment, and potentially even curing certain types of cancer. By harnessing the power of the immune system, these vaccines provide a targeted approach to combat cancer with fewer side effects compared to conventional vaccines.
As exploration progresses, the hope is that cancer vaccines will become a standard part of the oncologist’s toolkit, transforming the landscape of cancer treatment and offering new hope to patients worldwide. The intertwining roles of antigens and antibodies in this context underline the sophisticated and precise nature of these revolutionary therapies.
Reference
1 Coulie PG, Hanagiri T, Takanoyama M: From Tumor Antigens to Immunotherapy. Int J Clin Oncol 6:163, 2001.